
Date: 06 May 2025
Managing diabetes isn’t just about monitoring your blood sugar it’s also about caring for the parts of your body most vulnerable to complications. Among the most affected? Your feet. Diabetes can silently damage nerves and blood vessels, especially in your lower limbs, making small foot problems potentially serious.
Without proper foot care, people living with diabetes face a higher risk of infections, ulcers, and even amputations. But with a simple daily routine and the right diabetic footcare products, you can stay ahead of these risks and keep your feet healthy, soft, and strong.
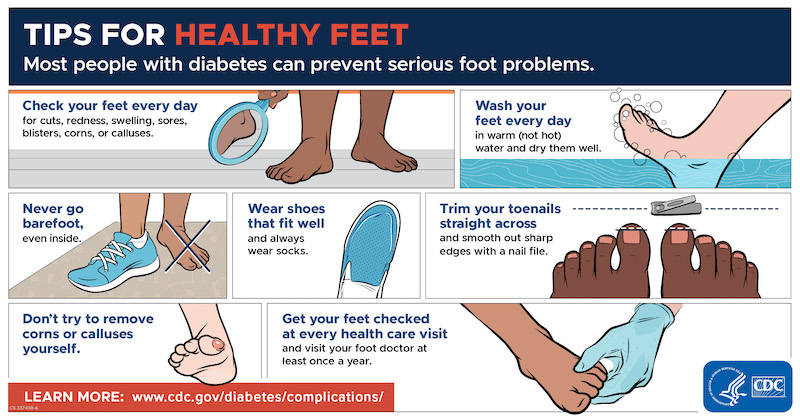
Foot injuries in diabetic patients often go unnoticed because of reduced sensation caused by neuropathy. That’s why a daily visual inspection is non-negotiable. Look for cuts, blisters, swelling, or changes in skin color these can signal infections or circulatory problems early on.
Checking your feet daily allows you to spot and treat minor problems before they escalate into serious infections. Use a mirror or ask for help if necessary you don’t want to miss a hidden sore between the toes or under the sole.
Hygiene is a key part of diabetic footcare. Washing your feet every day helps remove dirt, bacteria, and sweat that can irritate or infect your skin. Use lukewarm water—never hot—to avoid accidental burns due to reduced foot sensitivity.
Choose a mild, fragrance-free soap to prevent skin irritation. After washing, make sure to pat your feet dry, especially between the toes, where moisture can promote fungal growth.
Dry, cracked skin is common in people with diabetes due to reduced oil production and circulation. Moisturizing your feet daily keeps the skin soft and hydrated, reducing the risk of painful fissures that can lead to infections.
However, avoid applying lotion between your toes. Excess moisture in those areas creates a perfect breeding ground for bacteria and fungi. Use a foot cream designed for diabetics for best results.
Improper nail trimming can lead to ingrown toenails, infections, and sores—especially dangerous if you have diabetes. Use clean nail clippers and cut your toenails straight across to prevent the edges from digging into your skin.
If your nails are thickened, hard to cut, or you can’t reach them safely, consider visiting a podiatrist. It’s better to ask for professional help than risk a painful injury.
Wearing the right shoes is one of the best ways to protect diabetic feet. Choose closed-toe, cushioned shoes that fit well and reduce friction. Avoid tight footwear, sandals, and walking barefoot—even indoors.
Pair your shoes with diabetic socks made from moisture-wicking, seamless fabric. These socks reduce pressure points, improve circulation, and keep your feet dry and comfortable all day.
Trying to remove corns or calluses yourself using sharp tools or harsh chemicals can easily damage your skin and cause infections. This is especially risky for diabetics with poor healing and low sensation.
Instead, consult a healthcare professional or podiatrist for safe removal. If you develop a blister or sore, cover it with a sterile dressing and seek medical attention if it doesn't improve.
Don’t ignore any unusual symptoms or signs of infection. If you notice open wounds, excessive swelling, pus, or a foul odor from your foot, seek medical attention immediately. These are often signs that a simple issue has progressed into a dangerous infection.
Other red flags include a change in skin color, persistent pain, or numbness that worsens over time. Seeing a podiatrist regularly for foot checkups is a proactive way to stay ahead of potential complications.
Consistently high blood glucose can damage blood vessels and nerves in your feet. By maintaining good glycemic control, you support proper circulation and reduce your risk of neuropathy and slow-healing wounds.
Use a glucometer regularly and follow your prescribed diet and medications to stay within your target range.
Gentle activities like walking, swimming, or yoga improve blood flow to your legs and feet. Better circulation means faster healing and reduced risk of foot ulcers.
Try to move for at least 30 minutes daily, even if it’s broken into short walks throughout the day. Always wear proper footwear while exercising.
Smoking narrows your blood vessels and restricts circulation to your feet—making healing more difficult and increasing your risk of complications. If you smoke, quitting is one of the best decisions you can make for your foot health.
At Pharmily, we understand how important it is to protect your feet when living with diabetes. That’s why we stock high-quality diabetic footcare products designed to support your daily routine, including:
✅ 100% authentic products
✅ Reliable home delivery across Kenya
✅ Affordable prices on essential health items
A: Yes. Diabetes can lead to nerve damage (neuropathy) and poor blood flow, increasing your risk for infections, ulcers, and even amputations if foot problems aren’t treated early.
A: People with diabetes should have a foot check at least once a year. If you have any history of ulcers, deformities, or neuropathy, you may need more frequent visits.
A: Clean the wound gently, cover it with a sterile bandage, and monitor for signs of infection. If it doesn’t begin to heal within a day or two, contact a healthcare professional immediately.